



- Partners
- …
- Partners



- Partners
- …
- Partners

Cancer Immunotherapy
New medicine and more hope
The immune system is a complex network of molecules, cells, organs and lymph tissues working together to defend the body against germs, cancer cells and other invaders. Lymphocytes (part of white blood cells) are a significant part of the immune system. They develop in the bone marrow from lymphoblasts (immature cells found in bone marrow). Lymphoblasts mature into infection-fighting cells called B-lymphocytes (B-cells) and T-lymphocytes (T-cells) in lymph tissues.
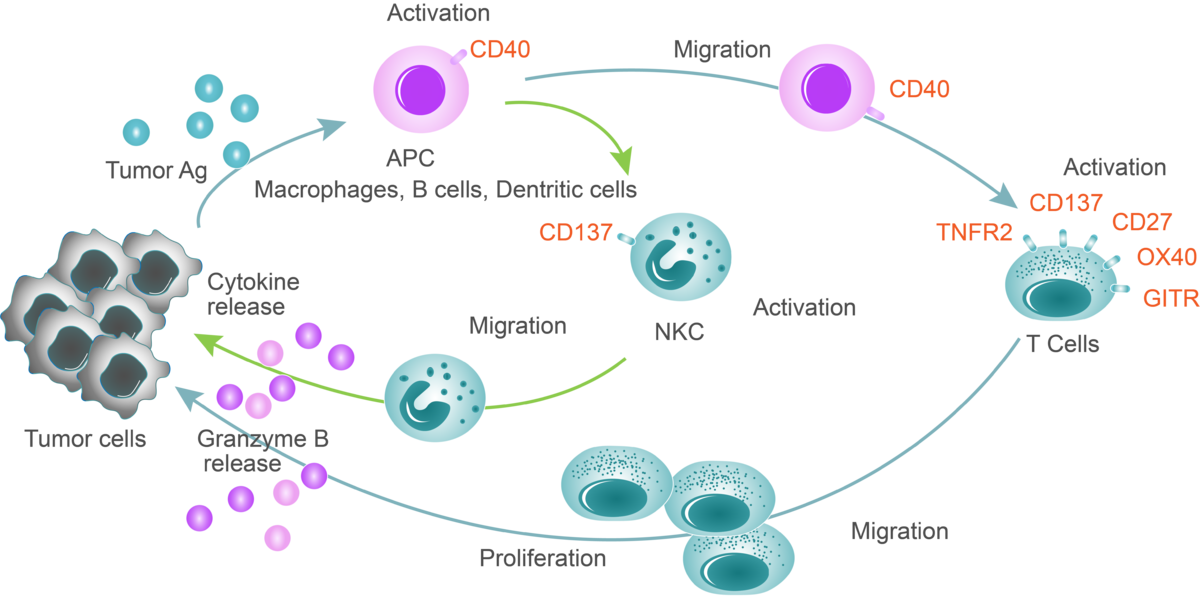
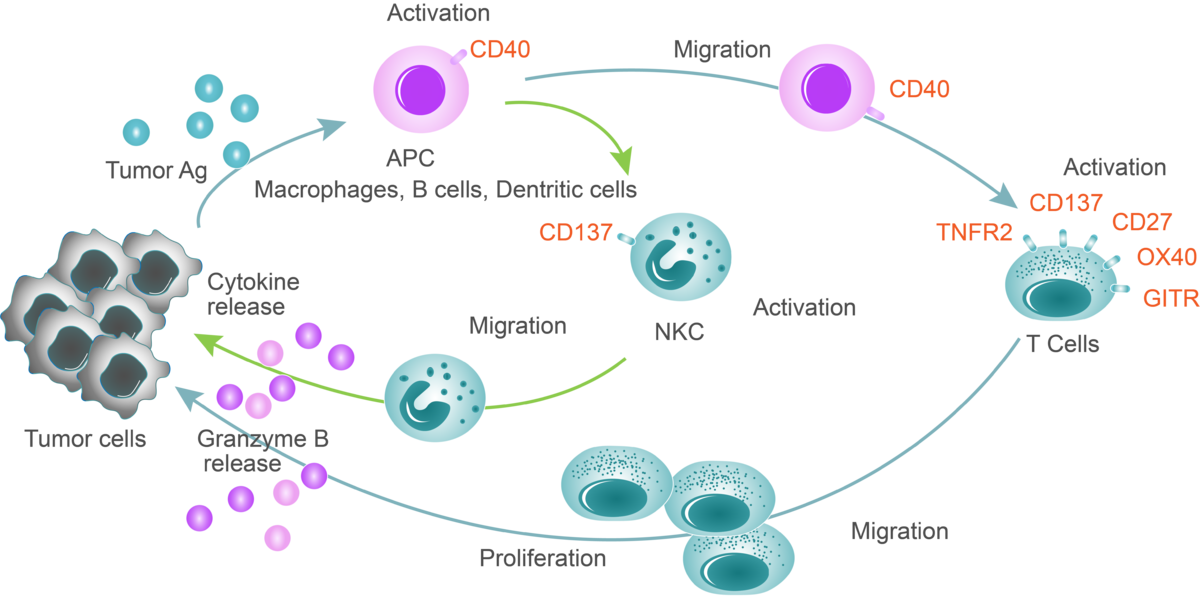
The immune system uses the same process to recognize and eliminate cancer as it does to remove other non-self cells. But the process is more complicated because cancer cells are created from normal cells by the body, so the normal ways to find and fight invading cells from outside the body aren’t always effective. The normal process for an immune response begins when dendritic cells, B-cells and helper T-cells identify the threat and tell the rest of the immune system. The body then ramps up its production of T-cells to fight. Killer T-cells can be activated by CD3 and co-stimulatory checkpoints. They are then sent to destroy the non-self cells. To prevent the T-cells from attacking healthy parts of the body, co-inhibitory checkpoint molecules and pathways, and regulatory T-cells are sent to slow the immune system down once the non-self cells have been eliminated. As a result, the body slows production of T-cells, which then return to normal levels.
Cancer develops when one or several abnormal cells divide and multiply to become a mass (tumor). The tumor may become different enough from the body that the immune system recognizes it as non-self and stimulates an immune response. However, the immune system may have difficulty identifying cancer cells as non-self. It may still see them as part of the body and not coordinate an attack. If the body can’t tell the difference between tumor cells and normal cells, the tumor cells may be able to “hide” and evade the immune system. The longer the cancer cells face a weakened immune response, the more they’re able to adapt, and the easier it is for them to manipulate immune cells inside the tumor’s location, sometimes called the micro-environment area.
Immunotherapy offers the immune system reinforcements to keep up its fight, whether that is through taking the brakes off the system or boosting it directly with stimulators such as our candidate agonist antibodies.
Co-stimulatory and co-inhibitory checkpoints keep the immune system “in check,” stimulating it to fight cancer and preventing an attack on normal cells in the meantime. When the correct proteins and cell receptors connect, a series of signals is sent to the immune system to boost or slow down an immune response.
We are developing antibodies targeting these co-stimulatory and co-inhibitory checkpoints for better cancer treatment. Tumor necrosis factor receptor superfamily (TNFRSF) members such as CD40, OX40 and CD137/4-1BB are expressed on myeloid cells and/or lymphocytes, and they regulate antigen presentation and adaptive immune activities. Our most advanced candidate antibodies have already entered the clinical development: anti-CD40 (LVGN7409), anti-CD137 (LVGN6051), and anti-PD-1 (LVGN3616).
If you as a patient or caregiver wish to participate in our clinical studies, please find more information by clicking on the above projects (in orange) or contact us at the following address: clinical@lyvgen.com or send us a message.
 在此处添加文本段落
在此处添加文本段落
Lyvgen Biopharma Website 礼进生物 英文官网
Lyvgen is a biotech company focused on developing novel therapies for cancer. Lyvgen’s xLinkAb™ functional platform creates agonist antibodies (Abs) with tumor-localized immunostimulatory activities by balancing multiple functions of candidate Abs.
https://user-assets.sxlcdn.com/images/676507/FiTA8WK-FQRyXrQDyd-HDkY3tpfI.png?imageMogr2/strip/auto-orient/thumbnail/1200x630>/format/png
 沪公网安备 31011502015346号
沪公网安备 31011502015346号